Detailed information on specific MSK (Muscular-Skeletal) conditions, such as Tendinopathies, which may require specialist treatment with Radial and/or Focused Shockwave Therapy.
3 - 6 sessions are generally required to heal most MSK cases for the average person who attends our clinic. The majority of patients report complete pain relief after 3-6 sessions and the rest mostly feel a significant pain reduction after this time. Radial and Focused Shockwave therapy helps to restore mobility and decrease pain quickly like no other non-invasive treatment on the market and therefore improving your quality of life and getting you back to doing the things you want to do - such as exercising/training with no invasive procedures.
Even in the most chronic of cases - such as long standing tendonitis, frozen shoulders etc. Shockwave therapy has an overall success rate of up to 90% successful, and that is even where other therapies like massage etc. have been already proven unsuccessful in helping.
Shockwave therapy can be used for a very wide range of different soft tissue ailments including common conditions like Achilles tendonitis, Plantar fasciitis, Hip bursitis (GTPS) and Tennis elbow but it is also very effective for more complicated issues like those that involving bones and joints such as stress fractures, non-union fractures, facet joints in the lower back and sacroiliac pain around the pelvis and spine.
Below is more detailed information on the most common MSK (Muscular-Skeletal) conditions that we see patients in clinic with on a regular basis.
Plantar Fasciitis.
Plantar fasciitis is a common condition that causes pain in the heel underneath the foot, due to inflammation or degeneration of the plantar fascia — a thick band of connective tissue that runs from the heel bone (calcaneus) to the toes.
-
It's a strong, fibrous ligament that supports the arch of your foot.
-
Acts like a shock absorber during walking, running, and standing.
-
When overstressed, it can become inflamed or develop tiny tears, which can cause pain and in severe instances, can stop you from being able to walk properly.
3. Stimulates tissue healing
-
The microtrauma from shockwaves triggers the body’s natural repair response.
-
Growth factors are released, helping cells rebuild and reorganise the damaged Plantar Fascia.
-
Collagen production is increased, which strengthens the fascia.
4. Breaks up scar tissue & calcifications
-
In chronic Plantar Fasciitis, the fascia can develop tiny areas of degeneration or calcification.
-
Shockwaves help break down disorganised scar tissue, restoring normal structure and elasticity.
5. Improves function
-
With reduced pain and better tissue healing, people often experience:
-
Less morning heel pain
-
Easier walking and standing
-
Faster return to normal activities and playing sports
-


PF is often caused due to repetitive strain or excessive load on the plantar fascia. Common risk factors include:
-
Overuse (especially running, jumping, or standing for long periods)
-
Tight calf muscles or Achilles tendon
-
Flat feet or high arches
-
Improper footwear (unsupportive shoes or barefoot walking on hard surfaces)
-
Sudden weight gain
Symptoms include;
-
Sharp, stabbing heel pain, especially:
-
First thing in the morning (first steps out of bed)
-
After prolonged sitting or standing
-
After exercise (but usually not during)
-
-
Tenderness at the bottom of the heel
-
Tightness in the arch or calf
How Shockwave Therapy helps with Plantar Fasciitis.
1. Increases blood flow
-
Plantar fascia tissue has poor blood supply, which slows healing.
-
Shockwave Therapy targets the injured tissue and cause microtrauma that stimulates the body to form new blood vessels (neovascularization).
-
This brings more oxygen and nutrients to the damaged fascia, speeding up repair.
2. Reduces pain
-
Shockwaves temporarily desensitise nerve endings, lowering pain signals from the heel.
-
They also cause the release of natural pain-relieving chemicals (endorphins).
-
This reduces chronic pain without relying on medication.
Achilles Tendonitis.
Achilles tendonitis is a condition that involves inflammation or irritation of the Achilles tendon, which is the large tendon that connects the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). This tendon is essential for walking, running, and jumping.
Achilles tendonitis is usually caused by overuse or repetitive stress, especially from activities that involve:
-
Running (especially uphill or on hard surfaces)
-
Sudden increase in activity level
-
Tight or weak calf muscles
-
Improper footwear
-
Poor running mechanics
There are two main types:
-
Non-insertional Achilles tendonitis:
-
Affects the middle portion of the tendon.
-
Common in younger, active people.
-
Tendon fibers begin to degenerate and thicken.
-
-
-
Insertional Achilles tendonitis:
-
Affects the lower part of the tendon where it attaches to the heel bone.
-
Can occur in anyone, even those who are not active.
-
Sometimes associated with bone spurs.
-
-
Pain and stiffness in the back of the heel or lower calf
-
Pain that worsens with activity
-
Swelling or thickening of the tendon
-
Tenderness when touched
-
Limited range of motion in the ankle
-
A creaking or crackling feeling (crepitus)


How Shockwave Therapy helps with Achilles Tendonitis.
1. Increases blood flow
-
The Achilles tissue has poor blood supply, which slows healing.
-
Shockwave Therapy targets the injured tissue and cause microtrauma that stimulates the body to form new blood vessels (neovascularization).
-
This brings more oxygen and nutrients to the damaged tissue, speeding up repair.
2. Reduces pain
-
Shockwaves temporarily desensitise nerve endings, lowering pain signals from the heel.
-
They also cause the release of natural pain-relieving chemicals (endorphins).
-
This reduces chronic pain without relying on medication.
3. Stimulates tissue healing
-
The microtrauma from shockwaves triggers the body’s natural repair response.
-
Growth factors are released, helping cells rebuild and reorganise the damaged Plantar Fascia.
-
Collagen production is increased, which strengthens the tissue.

4. Breaks up scar tissue & calcifications
-
In chronic Achilles Tendinitis, the Achilles can develop tiny areas of degeneration or calcification.
-
Shockwaves help break down disorganised scar tissue, restoring normal structure and elasticity.
5. Improves function
-
With reduced pain and better tissue healing, people often experience:
-
Less morning heel pain
-
Easier walking and standing
-
Faster return to normal activities and playing sports
-
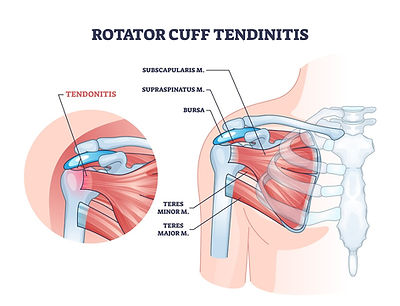
Shoulder Tendonitis.
Shoulder tendonitis (sometimes called rotator cuff tendonitis or biceps tendonitis, depending on which tendon is affected) is an inflammation or irritation of the tendons in the shoulder.
A tendon is a tough cord of fibrous tissue that connects muscle to bone. In the shoulder, tendons help stabilize the joint and allow you to lift, rotate, and move your arm. When these tendons become irritated or inflamed, it causes pain and reduced mobility.
Common Causes;
-
Overuse or repetitive movements (e.g., throwing, swimming, painting, lifting overhead)
-
Injury or strain
-
Poor posture (slouching or forward head posture puts strain on the shoulder)
-
Age-related wear and tear (tendons lose elasticity and blood supply over time)

Symptoms include;
-
Dull or aching pain in the shoulder, especially with movement
-
Pain at night (often when lying on the affected side)
-
Swelling or tenderness around the joint
-
Limited range of motion or weakness when lifting or rotating the arm
If untreated, shoulder tendonitis can progress to tendinosis (chronic degeneration) or contribute to rotator cuff tears.
How Shockwave Therapy helps with Shoulder Tendonitis.
1. Stimulates healing in the tendon
-
Shoulder tendinitis often involves degeneration (tendinopathy) rather than just simple inflammation.
-
Shockwaves create microtrauma in the tendon, which:
-
Increases local blood flow
-
Triggers the release of growth factors
-
Boosts collagen production, helping the tendon repair itself
-
2. Reduces pain
-
Shockwaves temporarily desensitize pain nerves in the shoulder.
-
They also stimulate the release of endorphins, the body’s natural pain relievers.
-
This means patients often feel less pain even before the tendon fully heals.
3. Breaks down calcifications
-
In calcific tendonitis of the shoulder (common in the supraspinatus tendon), calcium deposits can cause severe pain and stiffness.
-
Shockwave therapy helps fragment and dissolve these calcific deposits, making it easier for the body to reabsorb them.
4. Improves shoulder function
-
With pain reduced and tissue healing stimulated, patients usually notice:
-
Less pain at night (common with shoulder tendinitis)
-
Improved range of motion
-
Easier overhead movements
-
.jpeg)

Tennis Elbow (Lateral Epicondylitis)
Tennis elbow (medical term: lateral epicondylitis) is a condition where the tendons that attach to the outside of your elbow become irritated or inflamed, usually from overuse. Despite the name, it’s not limited to tennis players—any repetitive gripping or wrist/forearm activity can cause it.
What’s Happening
-
The pain comes from tiny tears and degeneration in the tendon that attaches forearm muscles (mainly the extensor carpi radialis brevis) to the bony bump on the outside of your elbow (lateral epicondyle).
-
These muscles help you extend (straighten) your wrist and fingers.

Common Causes
-
Repetitive wrist and arm motions (sports, typing, painting, carpentry, using tools, even frequent texting).
-
Gripping or twisting activities (e.g., turning a screwdriver, carrying heavy grocery bags).
-
Overuse without enough recovery time.
Symptoms
-
Pain or burning on the outside of the elbow.
-
Weak grip strength.
-
Pain that worsens with shaking hands, turning a doorknob, or lifting objects with the palm facing down.
-
Sometimes pain radiates down the forearm.
How Shockwave Therapy helps with Tennis elbow.
1. Stimulates tendon healing
-
Tennis elbow involves degeneration and microtears of the forearm extensor tendon (not just inflammation).
-
Shockwave therapy creates controlled microtrauma in the tendon, which:
-
Increases blood flow to the poorly vascularized tendon
-
Promotes release of growth factors
-
Stimulates collagen production and tendon repair
-
2. Reduces Pain
-
Shockwaves desensitize local pain nerves, reducing their ability to send pain signals.
-
They also trigger the release of natural pain-relieving chemicals (endorphins).
-
This provides both short-term pain relief and helps patients tolerate rehab exercises.

3. Breaks up scar tissue & adhesions
-
Chronic tennis elbow can lead to disorganized scar tissue at the tendon’s attachment on the lateral epicondyle.
-
Shockwaves help disrupt adhesions and restore more normal tendon structure, improving flexibility and function.
4. Improves function over time
-
With pain reduced and tendon healing stimulated, patients usually notice:
-
Stronger grip strength
-
Less pain during daily activities (shaking hands, lifting, gripping)
-
Better tolerance for exercise and sport
-
Osteoarthritis (OA).
Osteoarthritis (OA) is the most common form of arthritis. It’s a degenerative joint disease where the protective cartilage that cushions the ends of your bones gradually wears down. Over time, this leads to pain, stiffness, and reduced joint mobility.
What Happens in OA
-
Cartilage breakdown: The smooth, slippery cartilage covering the ends of bones becomes thin and rough.
-
Bone changes: Bones may rub directly against each other, causing pain and damage. Small bony growths called bone spurs (osteophytes) may form.
-
Joint inflammation: The lining of the joint (synovium) can become irritated, contributing to swelling and pain.
-
Commonly Affected Joints
-
Knees
-
Hips
-
Hands and fingers
-
Spine (neck or lower back)
-
Symptoms
-
Joint pain that worsens with activity and improves with rest
-
Stiffness, especially in the morning or after sitting still
-
Reduced flexibility or range of motion
-
Swelling around the joint
-
Clicking, grating, or “locking” sensations
Risk Factors
-
Age (risk increases with age)
-
Genetics (family history)
-
Joint injuries or overuse
-
Obesity (extra weight adds stress on joints, especially knees/hips)
-
Gender (women are more likely to develop OA after age 50)
Lateral hip pain / Bursitis (GTPS)
GTPS stands for Greater Trochanteric Pain Syndrome.
It’s a condition that causes pain on the outer (lateral) side of the hip, around the greater trochanter (the bony bump on the upper thigh bone/femur where muscles and tendons attach).
What’s Happening in GTPS
GTPS is not just one problem—it’s an umbrella term that includes:
-
Gluteal tendon irritation or tears (especially gluteus medius/minimus tendons)
-
Trochanteric bursitis (inflammation of the fluid-filled sacs that cushion the hip)
-
Muscle imbalances or tightness around the hip and pelvis
Symptoms
-
Pain on the outside of the hip or thigh, sometimes radiating down the outer leg
-
Worse when lying on the affected side (common night pain)
-
Pain with walking, climbing stairs, or standing on one leg
-
Tenderness when pressing on the outer hip
Risk Factors
-
More common in women, especially ages 40–60
-
Repetitive movements (running, cycling, prolonged standing)
-
Hip muscle weakness or imbalance
-
Lower back or pelvic alignment issues
-
Obesity (extra stress on hip structures)
Frozen Shoulder.
Frozen shoulder (medical term: adhesive capsulitis) is a condition where the shoulder joint becomes stiff, painful, and loses its normal range of motion. It happens when the capsule of connective tissue surrounding the shoulder joint thickens and tightens, restricting movement.
Key Features
-
Pain: Usually a dull, aching pain in the shoulder (sometimes in the upper arm too).
-
Stiffness: Difficulty raising, rotating, or moving the arm.
-
Loss of motion: Everyday tasks (like reaching overhead, dressing, or fastening a bra) become hard.
Stages of Frozen Shoulder
-
Freezing stage (painful stage)
-
Lasts ~2–9 months
-
Gradually worsening pain and stiffness
-
-
Frozen stage (stiff stage)
-
Lasts ~4–12 months
-
Pain may ease, but movement is very limited
-
-
Thawing stage (recovery stage)
-
Lasts ~6 months to 2 years
-
Shoulder motion slowly improves
-
Causes & Risk Factors
Often the cause is unknown, but risks include:
-
Injury or immobilization (e.g., after surgery or a fracture)
-
Diabetes (much more common in people with diabetes)
-
Thyroid problems
-
Age 40–60
-
Women are affected more often than men
Patella Tendonitis (Jumper's Knee)
Patellar tendonitis (also called Jumper’s Knee) is an overuse injury affecting the patellar tendon — the thick cord of tissue connecting your kneecap (patella) to your shinbone (tibia). It plays a key role in knee extension, especially during jumping, running, or squatting.
Causes
The main cause is repetitive stress on the patellar tendon, leading to tiny tears and inflammation. Over time, if left untreated, this can progress to tendinosis (degeneration without inflammation).
Common contributing factors:
-
Repetitive jumping or running (especially on hard surfaces)
-
Poor landing mechanics
-
Weak or tight quadriceps and hamstrings
-
Sudden increase in training load or intensity
-
Muscle imbalances or poor mobility
-
Inadequate recovery
Symptoms
-
Pain below the kneecap (where the tendon attaches)
-
Worse with activity, especially jumping or stairs
-
Tenderness to touch
-
Stiffness in the knee (especially after rest or first thing in the morning)
-
Swelling may be present in early stages

Proximal Hamstring Tendinopathy (PHT)
Proximal hamstring tendinopathy (PHT) is a condition where the tendons of the hamstring muscles become irritated or degenerated at their origin point on the ischial tuberosity (the “sit bone” at the bottom of your pelvis).
Instead of acute inflammation (like in tendonitis), it’s usually more of a chronic overload and degeneration problem (tendinopathy).
What’s Happening
-
The hamstrings (group of 3 muscles at the back of the thigh) attach high up on the pelvis.
-
With repetitive stress, overuse, or sudden load increases, the tendon fibers can develop microscopic damage.
-
Unlike a tear, it’s usually a slow, nagging condition that builds over time.
Symptoms
-
Deep buttock pain (near the sit bone), sometimes radiating down the back of the thigh.
-
Pain worsens with activities that stretch or load the hamstrings:
-
Running (especially sprinting or uphill)
-
Prolonged sitting
-
Bending forward from the hips
-
-
Tenderness when pressing near the sit bone.
Risk Factors
-
Runners, sprinters, dancers, and athletes in kicking sports.
-
Sudden increases in training load or intensity.
-
Weakness or poor flexibility in hamstrings or glutes.
-
Poor pelvic or hip mechanics.
Shin Splints (MTSS)
Medial Tibial Stress Syndrome (MTSS) — often called “shin splints” — is an overuse injury that causes pain along the inner (medial) edge of the shinbone (tibia). It happens when the muscles, tendons, and bone tissue around the tibia are overloaded.
What’s Happening
-
Repetitive stress (often from running, jumping, or sudden activity increases) causes microtrauma to the muscles and tendons that attach to the tibia.
-
The bone itself may also develop stress reactions (early stages of a stress fracture if left untreated).
Symptoms
-
Dull, aching pain along the inner shin, usually in the lower 1/3 of the tibia.
-
Pain that:
-
Starts with exercise, improves during activity, but worsens after
-
In later stages, may hurt even at rest
-
-
Tenderness when pressing along the inner shin.
-
Mild swelling sometimes present.
Risk Factors
-
Sudden increase in running distance, speed, or intensity
-
Running on hard or uneven surfaces
-
Flat feet (overpronation) or very high arches
-
Inadequate footwear
-
Weak calf or hip muscles
-
Sports with repetitive impact (running, basketball, soccer, military training)
Patellofemoral Pain Syndrome (Runner's Knee)
Patellofemoral Pain Syndrome (PFPS) — often called “runner’s knee” — is a condition where you feel pain around or behind the kneecap (patella), especially during activities that load the front of the knee.
It’s one of the most common causes of knee pain, particularly in athletes and active individuals.
What’s Happening
-
The kneecap normally glides smoothly in a groove on the thigh bone (femur).
-
In PFPS, there’s irritation of the soft tissues around the patella due to abnormal movement (maltracking), overuse, or imbalances in muscle strength and flexibility.
-
Unlike arthritis or ligament injuries, there’s usually no structural damage, but pain can still be significant.
Symptoms
-
Dull, aching pain around or behind the kneecap
-
Pain worsens with:
-
Running, squatting, lunging
-
Climbing stairs (especially going down)
-
Sitting for long periods with knees bent (“theater sign”)
-
-
May feel grinding, clicking, or a sense of the knee “giving way”
-
Usually no major swelling (distinguishes it from other knee problems)
Risk Factors
-
Overuse or sudden increase in activity
-
Muscle imbalances (weak hip abductors, weak quads, or tight hamstrings/calves)
-
Flat feet or overpronation
-
Poor running technique or footwear
-
More common in teenagers and young adults, especially females
Lower back pain (Lumbar Facet Joint Pain)
Lower back facet joint pain (also called facet joint syndrome or facet arthropathy) is pain that comes from the facet joints — the small joints at the back of the spine that connect the vertebrae and guide movement.
What’s Happening
-
Each vertebra has two pairs of facet joints (one on each side).
-
These joints are lined with cartilage and surrounded by a capsule filled with fluid, allowing smooth motion.
-
With age, injury, or overuse, the cartilage can wear down, the capsule may become irritated, and the joint can become a pain source.
-
Pain signals may also come from nearby ligaments and nerves.
Symptoms
-
Localized low back pain, often on one or both sides of the spine
-
Pain that:
-
Worsens when leaning backward, twisting, or standing up straight
-
Improves when bending forward
-
-
Stiffness, especially in the morning or after sitting
-
Sometimes pain radiates into the buttocks or thighs, but usually not below the knee (which helps distinguish it from sciatica)
-
Tenderness over the affected joints when pressed
Causes & Risk Factors
-
Osteoarthritis (degeneration of cartilage in the facet joints)
-
Repetitive stress (heavy lifting, twisting)
-
Spinal injury or trauma
-
Poor posture
-
Age-related wear and tear
Golfers Elbow
Golfer’s elbow (medical term: medial epicondylitis) is a condition where the tendons on the inside of the elbow become irritated or damaged, leading to pain and tenderness.
It’s similar to tennis elbow, but the pain is on the inner (medial) side of the elbow rather than the outer side.
What’s Happening
-
The tendons that attach the forearm flexor muscles (the ones that bend your wrist and fingers) to the medial epicondyle (the bony bump on the inside of your elbow) develop tiny tears and degeneration.
-
This usually results from repetitive gripping, wrist flexion, or forearm rotation.
Symptoms
-
Pain and tenderness on the inner side of the elbow
-
Pain may radiate down the forearm to the wrist
-
Worsens with:
-
Gripping (e.g., golf clubs, tools, shaking hands)
-
Lifting or throwing
-
Flexing the wrist against resistance
-
-
Stiffness and sometimes weakness in the hand/wrist
-
Numbness/tingling in fingers (especially ring and little fingers) in some cases
Causes & Risk Factors
-
Repetitive activities: golfing, throwing sports, racket sports, weightlifting
-
Jobs involving gripping or wrist flexion (plumbers, carpenters, computer work)
-
Poor technique in sports or lifting
-
More common in people ages 40–60
